 |
||
| |
|
|
A closer look at medical expenses that drive the cost of claims
In the annual State of the Line released in May by NCCI Holdings, Inc., the President and CEO Stephen J. Klingel notes, “ NCCI’s short-term view of the (Workers’ Compensation) line is optimistic, but the long-term view remains cautionary due to a series of critical issues that continue to face the business. As always, in a cyclical, long tail line such as Workers’ Compensation insurance, we need to be mindful of those challenges that threaten to negatively impact our business.” One of the major areas of concern is the continued escalation of medical costs. In Workers’ Compensation, this is compounded by the problem of over-utilization of medical services.
According to a recent survey of more than 70 health insurers representing more than 100 million insured individuals prepared by Aon Consulting, the costs of providing health care are projected to rise from 10.7% to 11.2% in the next twelve months. Add to this the fact that in recent years, Workers’ Compensation medical claims severities have been increasing at a faster rate than medical inflation alone and that studies have shown Workers’ Compensation pays more than group health to treat comparable injuries, it is clear that medical cost benefits will continue to drive the costs of claims.
An NCCI study, "Measuring the Factors Driving Medical Severity: Price, Utilization, and the Mix", by Tanya Restrepo, Harry Shuford and Nathan Beaven examined the factors responsible for the ongoing escalation of medical severity in Workers’ Compensation claims. While price increases were a minor factor, the growth in the number of treatments was the key driver. Accounting for approximately a 35% increase in medical severities over the years studied is the markedly higher number of treatments within each diagnosis and a different mix of treatments across service categories. For example, there might be a shift from diagnostic radiology to complex diagnostic testing or complex surgery to physical therapy.
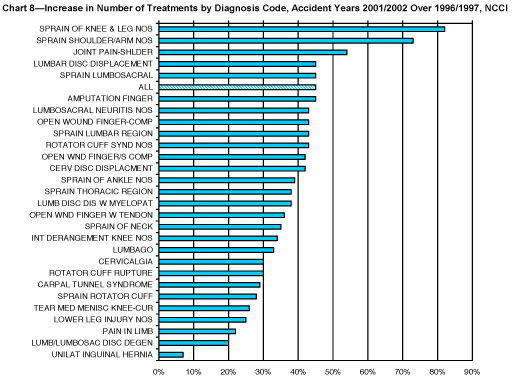
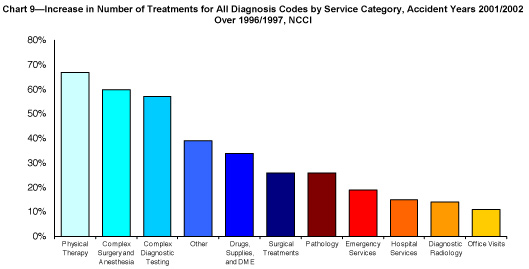
The following charts show the increase in the number of treatments by diagnosis code for the years 2001/2002 compared with 1996/1997.
NCCI Research Brief January 2007, Measuring the Factors Driving Medical Severity, Price, Utilization, Mix by Tanya Restrepo, Harry Shuford and Nathan Beaven.
The overall number of treatments increased for each of these diagnoses, ranging from an increase of 7% for unilateral inguinal hernia to more than 80% for sprain of knee and leg. For all diagnoses combined, the number of treatments increased 45%. Looking at the service categories, the three service groups with above average increases in the number of treatments over the study period were physical therapy (67%), complex surgery and anesthesia (60%) and complex diagnostic testing (57%).
An NCCI study comparing Group Health and Workers’ Compensation in 14 states from 1996 to 2004 also revealed that Workers’ Compensation pays more than group health to treat comparable injuries and that utilization differences explain 80% of the overall treatment cost difference. Chronic pain-related injuries such as bursitis, back pain and carpal tunnel have particularly large differences.
The results of these studies suggest that the primary factor propelling the upward trend in medical costs is changing patterns of utilization. Since utilization is a function of the injury, this highlights the value of injury specific cost controls aimed at over-utilization such as the application of evidence based guidelines.
Workers’ Compensation is a complex system and many parties contribute to medical decisions. While medical providers make initial testing, treatment and disability management decisions, claims adjusters, employers, nurse case managers, attorneys, and injured workers also make decisions about care and absence from work. These groups often use standards that are not based on evidence of effectiveness, but on a myriad of other factors, including traditional insurance industry practices, perceptions of regulations, threats of legal action, peer and family advice, and physician statements made without scientific evidence.
With the seismic shifts in medical innovation and the corresponding increase in treatment options and costs, providing appropriate, quality medical care requires a basis in scientific evidence. If the employer provides timely access to excellent medical care that uses objective, scientific-based guidelines to treat job-related injuries and focuses on a return to work, the employer and the employee benefit. Ensuring that quality and effectiveness drive your medical care selection criteria and communicating to the work force about the value in advance can go a long way in creating a positive response and controlling Workers’ Compensation costs.